Background
The SARS CoV-2 / COVID 19 pandemic has challenged the world's health systems, especially services that treat cancer. The first studies in China showed that cancer patients had a higher risk of becoming infected and dying. Other risk factors for mortality were age over 65 years, male sex, the presence of comorbidity, hypertension, cardiovascular disease, diabetes, and obesity. Data on the specific behavior of patients with multiple myeloma (MM) in the pandemic are scarce. The mechanisms by which MM patients may have a higher mortality are multiple, derived both from the disease itself due to cellular and humoral immunity deficiency as well as from anti-myeloma treatment. The present study aims to establish the behavior of the disease in the pandemic period in Latin America.
Methods
This is a retrospective case series of in and outpatients with a diagnosis of MM and COVID-19 reported from centers from Latin America between March and July 31, 2020. The analysis of demographic, clinical, laboratory, complications and therapy variables were done using descriptive statistics. A Kaplan Meier survival analysis was performed, with Log Rank statistic. Finally, a Cox regression was performed to identify independent risk factors of worse outcome. Pre-admission characteristics, MM status, and comorbidities constituted the reference model and were used to adjust the association of relevant MM characteristics with mortality. Program used for analysis was SPSS statistics 25.
Results
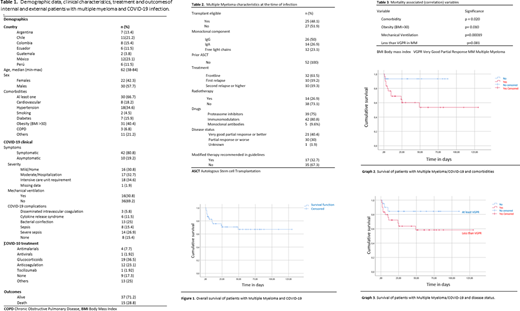
Fifty-two patients with COVID-19 and MM from 7 countries were included. Demographic characteristics, comorbidities, infection baseline clinical conditions, treatment, and outcomes are shown in Table 1. The characteristics in terms of MM status are shown in Table 2.
When performing the survival analysis, it is evidenced that the survival of the entire cohort at day 49 was 67% Figure 1. When we focus on patients with comorbidities, survival drops to 53.5% +/- 10.6 (CI 95% 53.4 - 99.4 and p value of 0.041) for the same day Figure 2. When performing the obesity analysis, a drop in survival of up to 39% was observed (95% CI 24.448 - 56.76, with p = 0.00001) Figure 3. Adjusted HR for obesity is 5,078 (95% CI 1,389-18,558, α0.014) and mechanical ventilation with a HR of 3,943 (95% CI - 1,296 - 11,998, α0.016)
When comparing patients with controlled MM (> PR) versus uncontrolled, the mortality rate was 84% versus 58% respectively (p = 0.109). Comorbidities (presence of either diabetes, arterial hypertension, cardiovascular disease, or "others"), obesity, need of mechanical ventilation, and <VGPR at the time of infection were independent factors of lower survival Table 3.
Conclusions
Patients with MM and COVID-19 has an overall mortality of approximately 30% and this is strongly influenced by the presence of comorbidities, uncontrolled disease and need of mechanical ventilation. Survival of patients without comorbidities and controlled disease is good, suggesting that this group of patients would not require modification of MM therapy. The main limitations of our study are its retrospective nature and the low number of patients. It must be highlighted that at the time of the analysis most of Latin American countries were still in the peak of the pandemic. Prospective studies are required to elucidate the behavior of these risk factors in mortality, to optimize the management of patients with MM in this period of the SARS CoV-2 / COVID-19 pandemic.
Peña:BindingSite: Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Sandoz: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Amgen: Speakers Bureau. Abello:Novartis: Consultancy, Honoraria; Amgen: Consultancy, Research Funding; Takeda: Honoraria, Research Funding; Dr. Reddy's: Consultancy, Research Funding; Abbvie: Consultancy, Research Funding. Idrobo:Abbvie: Honoraria, Speakers Bureau; Tecnofarma: Honoraria, Speakers Bureau; Takeda: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; Amgen: Honoraria, Speakers Bureau. Rojas:Novartis: Consultancy; Roche: Honoraria; Sandoz: Honoraria; Abbvie: Honoraria. Remaggi:Takeda: Honoraria; Raffo Argentina: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Gador Argentina: Research Funding; Amgen: Honoraria, Research Funding. Alvarado:Celgene: Speakers Bureau; Alexion: Speakers Bureau; Amgen: Speakers Bureau; Novartis: Speakers Bureau; Roche: Speakers Bureau. De la Peña-Celaya:Amgen: Speakers Bureau; Janssen: Speakers Bureau; Novartis: Speakers Bureau. Perez:Novartis: Speakers Bureau; Celgene: Speakers Bureau; Roche: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal